Fractional flow reserve (FFR) is a technique used in coronary catheterization to measure pressure differences across a coronary artery stenosis (narrowing, usually due to atherosclerosis) to determine the likelihood that the stenosis impedes oxygen delivery to the heart muscle (myocardial ischemia).
FFR is a novel and potentially clinically useful mathematical model for estimation of stenotic coronary artery atherosclerosis. Reliability/collaborative (easily reproducible) measurement between competing laboratories in measuring this essential metric remains muddled in a proprietary race to claim cardiac mathematics dedicated to risk in ischemic cardiac disease. Proprietary claims of cardiac mathematics have not been previously argued in patent law. The race towards ownership of proprietary claims in defining ischemic disease remains elusive. Legal precedents abound stating mathematics should not be burdened by patent law.
Fractional flow reserve is defined as the pressure after (distal to) a stenosis relative to the pressure before the stenosis. The result is an absolute number; an FFR of 0.80 means that a given stenosis causes a 20% drop in blood pressure. In other words, FFR expresses the maximal flow down a vessel in the presence of a stenosis compared to the maximal flow in the hypothetical absence of the stenosis.
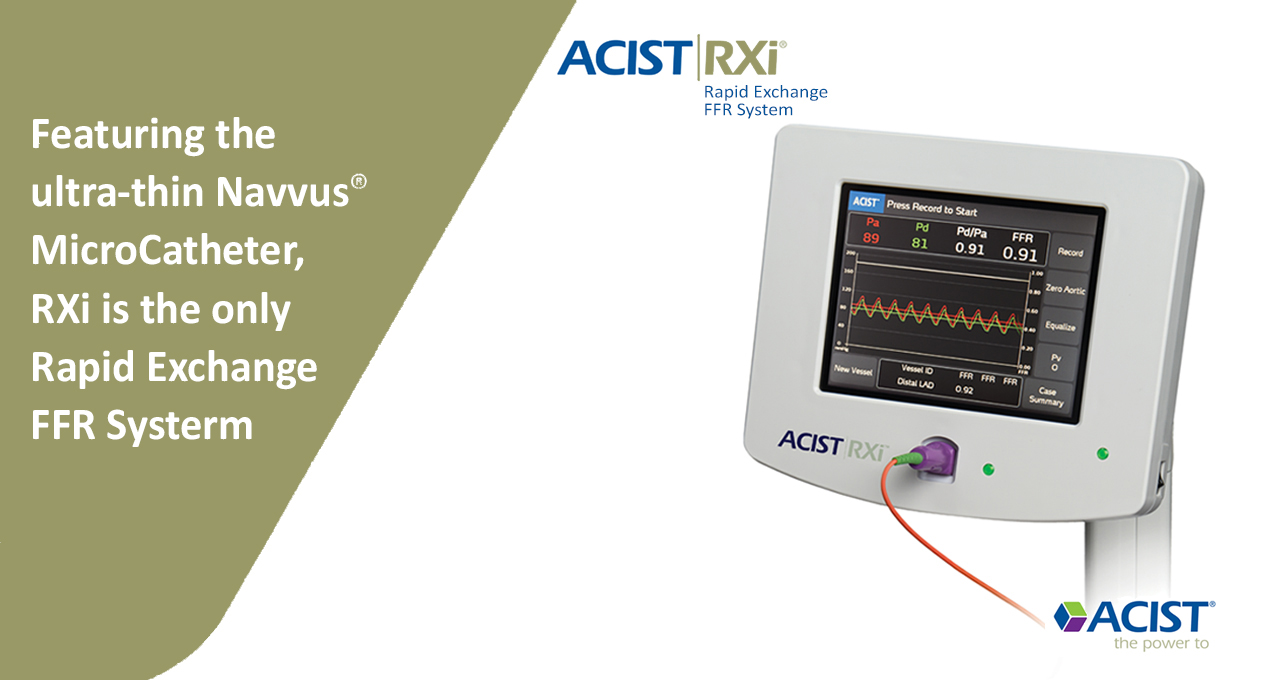
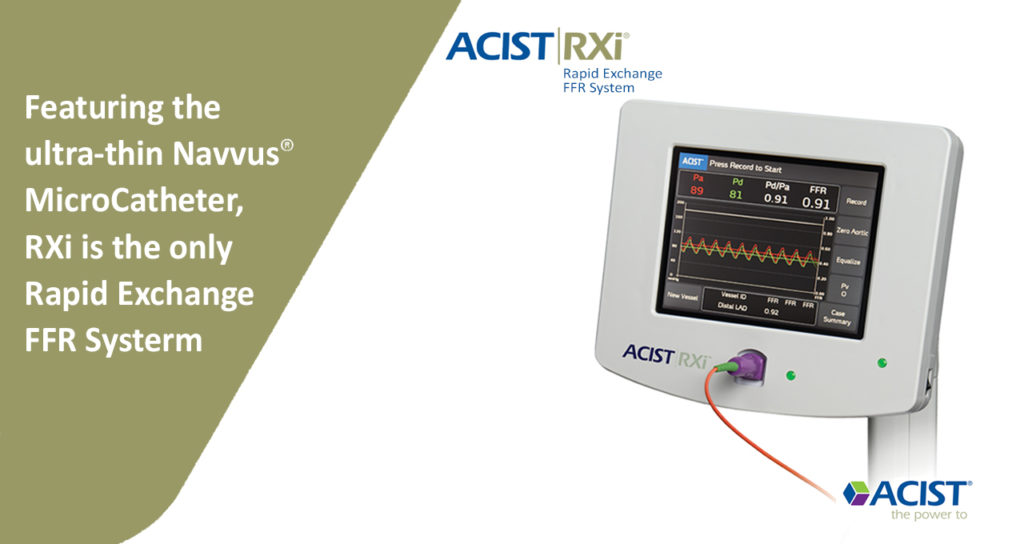
About RXi
The RXi system with the ultra-thin ACIST Navvus® Rapid Exchange FFR MicroCatheter gives you the freedom to quickly and easily assess FFR using your wire of choice.
Download Catalog
Benefits Of RXi
The RXi system does not require the use of a specialized guidewire. The Navvus MicroCatheter delivers over your 0.014˝ guidewire, providing you maximum control.
The RXi system allows wire position to be maintained even when performing pull-back assessments of multiple lesions. This also facilitates rapid FFR assessments before, during, and post-intervention.
The Navvus MicroCatheter uses fiber-optic sensor technology that provides accurate and reproducible hemodynamic pressure measurements. RXi produces accurate results with less drift when compared with traditional pressure-wire systems. In the ACCESS-NZ study, signal drift was significantly lower (0.02 vs 0.06; p=0.014) and clinically significant drift was observed in fewer measurements (13% vs 33%; p=0.022) with RXi than with a traditional system. Clinically significant drift is defined as > ±0.03.